Sleep was something you could rely on. But somewhere in your 40s, it may have begun to elude you. Suddenly, you're lying awake at 3 a.m., sweating profusely or fighting an active mind. Sound familiar?
You’re not alone. According to the National Sleep Foundation, upwards of 61% of women in perimenopause experience sleep issues. And it's not just why you feel tired — chronic sleep deprivation can affect everything from your mood and memory to your metabolism and hormones.
What is Perimenopause (and Why Is It Messing with Your Sleep)?
Perimenopause is the transition period leading up to menopause, typically starting in your 40s (occasionally even late 30s). Throughout this period, your ovaries reduce their production of estrogen and progesterone — hormones that control sleep, mood, temperature, and even your body's circadian rhythm.
These hormonal changes can lead to:
- Night sweats and hot flashes.
- Anxiety and mood swings
- Waking up multiple times per night
- restless legs or nighttime urination
The good news? These aren't forever — and they're treatable.
Here’s how you do that:
1. Balance Blood Sugar Before Bed
Hormonal fluctuations in perimenopause also increase insulin resistance, making you far more vulnerable to spikes and drops in your blood sugar, especially at night. A drop in blood sugar can trigger cortisol (your stress hormone) in the night, also waking you in the night.
Fix it: Eating a small bedtime snack of healthy fat, protein, and fiber.
Consider:
- A boiled egg and some almonds
- Greek yogurt with chia seeds
- A slice of avocado toast on whole grain bread
2. Make a Cool, Dark, Quiet Sleep Space
Perimenopausal women are more sensitive to outside stimuli such as noise and light. And those hot flashes? They're exacerbated by a hot bedroom.
Fix it:
- Make sure your room is between 60–67°F (15–19°C)
- Use blackout curtains or an eye mask
- Think about a white noise machine
- Sleep with light, moisture-wicking bedding
3. Don't Skip Movement, But Time it Right
Exercise decreases stress and balances hormones — but exercising late can get cortisol going and make it more difficult to fall asleep.
Fix it:
- Strive for morning or early afternoon activity
- Incorporate resistance exercises 2–3 times a week (excellent for bone health and mood)
- Add relaxing evening strolls or yoga to chill out
4. Establish a Regular Bedtime Routine
The circadian rhythm — your internal sleep-wake cycle — gets disrupted during perimenopause. A regular routine can reset it.
Try this wind-down routine:
- 8:30 PM: Shut off bright screens and overhead lights
- 9:00 PM: Warm bath or shower
- 9:30 PM: Light stretching or breathing
- 10:00 PM: Bedtime
5. Restrict Alcohol and Caffeine
Caffeine lingers in your system for 10 hours, and alcohol, which is relaxing initially, interferes with REM sleep and triggers 2 a.m. wake-ups.
Do this instead:
- Substitute evening wine with tart cherry juice (naturally increases melatonin)
- Swap coffee after noon with decaf or herbal tea (use chamomile, lemon balm, or rooibos)
Papayya provides a science-based supplement stack for enhanced sleep through hormonal transition. These are actual solutions, not snoozy hacks.
✅ All of the formulas are checked by functional health experts.
- A review of common dietary supplements for sleep quality, including melatonin, magnesium, zinc, vitamin D, and L-theanine
- Literature review on natural supplements such as melatonin, magnesium, and zinc improving sleep quality
- Review on hormonal changes and their impact on women's sleep during life transitions
- Study on sleep and sleep disorders in the menopausal transition and hormone therapy benefits
- Sleep supplement guide discussing evidence-based supplement combos for sleep
6. Say No to "Pushing Through"
Perimenopause isn't "a phase to push through." It's a physiological change that demands respect. Poor sleep isn't something to push through — it's something to mend.
That begins with improved habits, the proper equipment, and kindness to yourself.
7. Monitor Your Symptoms
A symptom journal may assist you in determining your personal sleep triggers. For instance:
- When did you last eat?
- Were you stressed out before bed?
- Was your bedroom too hot?
- Did you drink something?
Patterns show you what's actually happening — and get you in your rhythm.
8. Support Gut Health
Your gut and sleep are linked via the microbiome-hormone loop. Poor digestion → hormone imbalance → poor sleep.
Boost your gut:
- Add fermented foods such as kimchi, kefir, and yogurt
- Increase fiber (target 25g/day)
- Cut processed sugar and alcohol
9. Wear Weighted Blankets or Cooling Pillows
They might be gimmicky, but they're not. Weighted blankets can decrease nighttime anxiety by triggering deep pressure therapy. And cooling pillows are a night sweat game-changer.
Search for:
- 12-15lb weighted blankets for calming purposes
- Gel-infused or bamboo cooling pillows
10. Attack Anxiety Head-On
Anxiety is one of the biggest sleep interrupters in perimenopause. It's not "all in your head" — it's physiological. But don't despair.
Natural assistance includes:
- Adaptogenic botanicals (such as Rhodiola, holy basil)
- Physical movement on a regular basis
- Deep connection (even brief daily check-ins with pals)
11. Think about Cognitive Behavioral Therapy for Insomnia (CBT-I)
CBT-I is the gold standard for ongoing sleep problems. It rewires thinking and creates healthier sleep habits — all without medication.
You can search for certified therapists online or utilize CBT-I apps such as:
- Sleepio
- Somryst
- CBT-i Coach (free app)
12. Don't Stress About Being Perfect
It's easy to get caught up in perfect sleep, but that can work against you. Worrying about sleep keeps your body awake.
Instead:
- Celebrate small victories (such as one fewer wake-up)
- Take it easy on your body
- Understand healing is a slow process
13. Bonus: Discuss HRT or Non-Hormonal Options with Your Doctor
For other women, lifestyle adjustments aren't sufficient — and that's fine. Hormone Replacement Therapy (HRT) or non-hormonal medication may be the way to go.
Always consult with a practitioner who is familiar with perimenopause. Perhaps a functional medicine physician or OB-GYN who has experience with midlife care.
Wellness isn’t a one-size-fits-all deal. Get a personalized plan that meets you where you are—try Papayya free for 7–14 days.
Key Points to Remember
1. Begin Your Day With Natural Light
One of the easiest but most neglected solutions for enhancing sleep quality is to reset your internal body clock—your circadian rhythm. Spending 10-15 minutes outside in natural sun about one hour after waking up can be magical. It tells your brain it's daytime, making your sleep-wake cycle regulate better at night.
2. Give CBT-I a shot If you are tired of tossing and turning
If late nights without sleep are now terrifyingly usual for you, you may need something more structured such as Cognitive Behavioral Therapy for Insomnia (CBT-I). It's less scary than it sounds—CBT-I merely teaches you to recognize and modify thoughts and behaviors that interfere with your sleep.
In contrast to sleep aids that cover up the problem, CBT-I addresses the core issue. You are taught useful strategies to decrease anxiety in bed, stop racing with the need to "try harder" to fall asleep, and exchange counterproductive habits (such as doom-scrolling in bed). Many apps and websites now provide CBT-I courses, so it has never been simpler to attain access—even if you're not prepared for face-to-face therapy.
3. Track Your Sleep Like You’d Track Your Period
You might already track your cycle or moods, why not sleep? By simply keeping a sleep log (even if just a note on your phone) over a couple of weeks may reveal some surprisingly useful correlations. For example, your most challenging nights may be preceded by a day of stress, a late dinner, or correlating to a period in your cycle.
I recommend you keep track of when you went to bed, when you woke up, what you ate, how you were feeling emotionally, as well as any hot flashes and/or night sweats. By the end of the week or two, you should be able to begin identifying some triggers. Awareness won't fix it, but it gives you control to make specific changes.
4. Nourish Your Gut to Nourish Your Sleep
It may be weird, but your sleep and your gut are more related than you realize. A healthy gut microbiome affects the production of serotonin—a hormone that not only impacts your mood, but also your sleep-wake cycle. Try incorporating more gut-friendly foods into your diet—like plain yogurt, kefir, bananas, oats, and fermented veggies.
Want to see how Papayya works in real life? Read real stories from real people—no filters, no fake hype.
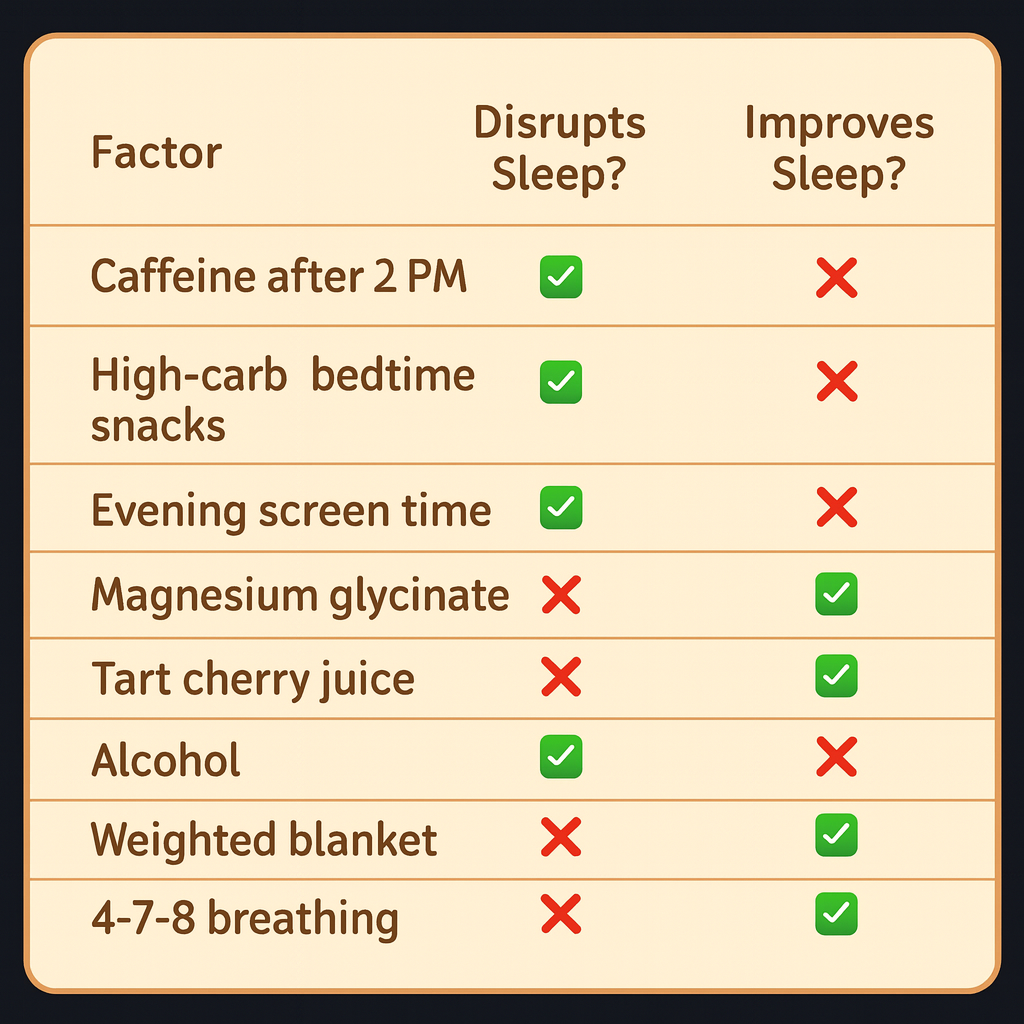
Comparison Chart: What Affects Perimenopausal Sleep
Final Word
Your sleep is important. Particularly now.
It's not egotistical to need to feel well-rested. It's crucial. And with the correct knowledge, guidance, and daily adjustments, your best sleep can still be in your future.
✨ To reset your sleep naturally? Begin your complimentary 7–14 day trial at Papayya.com
%20(1).png)
References
- CBT-I for Insomnia. National Sleep Foundation:
https://www.sleepfoundation.org/insomnia/treatment/cognitive-behavioral-therapy
- Morning Sunlight and Circadian Rhythm. NIH Study on Bright Light and Sleep:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6520878/
- Gut Health and Sleep. Cleveland Clinic on Gut-Brain Connection:
https://health.clevelandclinic.org/gut-brain-connection
- Menopause Sleep Disruptions. North American Menopause Society:
https://www.menopause.org/for-women/sleep-and-menopause
- Effectiveness of Herbal Remedies. NIH on Herbal Remedies for Sleep:
https://www.nccih.nih.gov/health/sleep-disorders
- The Role of Sleep Journals. Sleep Foundation on Keeping a Sleep Diary:
https://www.sleepfoundation.org/sleep-diary
.svg)

.webp)
 FACEBOOK
FACEBOOK
